measuring cesarean scar thickness|cesarean section scar measurement : distribute Result: Scar thickness was thinner in those patients having cesarean delivery than those having vaginal delivery and this difference was statistically significant at both the gestational ages. Mean scar thickness at 24-28 weeks of gestation in patients who delivered vaginally is 4.8 ± 1.1 mm and in those who had repeat cesarean section is 4.4 .
webVárias Queixas CIFRA Gilsons - Experimente o Banana Cifras e tenha acesso grátis a milhões de cifras para tornar suas sessões musicais ainda mais incríveis.
{plog:ftitle_list}
WEB10/08/2021 - 10:33hs BRT. A Rede Record foi condenada pela Justiça de São Paulo a pagar uma indenização no valor de R$ 50 mil ao YouTuber Maicon Küster por danos .
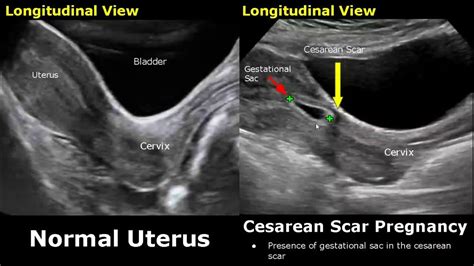
Here, we review the literature regarding third-trimester ultrasonographic assessment of uterine scar in the evaluation of the risk of uterine rupture following previous .Key sonographic markers, including gestational sac location, cardiac activity, placental implantation and myometrial thickness, are detailed. The evaluation process is presented . Scar thickness from 3.0 to 3.5 mm was found in 36% of cases, of which 18% of cases of scar separation is found. The study concluded that the lower uterine segment . The integrity and thickness of the previous cesarean section scar of the lower uterine segment (LUS) assessed by ultrasound is a popular strategy that has been proposed to estimate the likelihood of uterine rupture or dehiscence that might occur spontaneously or during labor trial; this can be done alone or in combination with clinical factors .
uterus scar size after cesarean section
ultrasound for cesarean section scar
Background and Objectives: To investigate the prevalence of a Cesarean section (CS) scar niche during pregnancy, assessed by transvaginal ultrasound imaging, and to relate scar measurements, demographic and obstetric variables to the niche evolution and final pregnancy outcome.Materials and Methods: In this prospective observational study, we used . Result: Scar thickness was thinner in those patients having cesarean delivery than those having vaginal delivery and this difference was statistically significant at both the gestational ages. Mean scar thickness at 24-28 weeks of gestation in patients who delivered vaginally is 4.8 ± 1.1 mm and in those who had repeat cesarean section is 4.4 .
Background and Objectives: The aim of this study is to evaluate changes in uterine scar thickness after previous cesarean delivery longitudinally during pregnancy, and to correlate cesarean section (CS) scar myometrial thickness in the first trimester in two participants groups (CS scar with a niche and CS scar without a niche) with the low uterine segment (LUS) .
Study also showed that scar thickness of 2.55mm and above measured by transabdominal method in the third trimester can be safely given trial of VBAC.Conclusions: Authors thus conclude that measurement of lower uterine segment/ scar thickness can help obstetrician decide whether VBAC is safe or not in patients with previous one LSCS willing for .
Introduction. A wedge-shaped hypoechoic Cesarean section (CS) scar was first described using hysterosalpingography in 1961 1, transabdominal sonography (TAS) in 1982 2 and transvaginal sonography (TVS) in 1990 3.The first two studies were in non-pregnant women and the third included both pregnant and non-pregnant populations. The method currently used to predict CS scar rupture is ultrasonographic measurement of the thickness of the lower uterine segment (LUS) in gestational week 36–38 as . Brölmann HA, Huirne JA, Timmerman D, Bourne T: Standardized approach for imaging and measuring Cesarean section scars using ultrasonography. Ultrasound Obstet Gynecol. 2012 .Discussion. In the current study, the entire lower segment thickness was measured from the muscularis and mucosa of the bladder on the outer side to the chorioamniotic membrane inside transabdominally using 2D and 3D ultrasound.The mean LUS thickness was 4.98±1.32 and 4.14±1.11 mm by 2D and 3D ultrasound, respectively.It has been reported that the thickness .
The study showed that ultrasound measurement of 3D ultrasound thick scar on the uterus after previous cesarean section has practical application in determining the mode of delivery among pregnant women who have previously given birth by Caesarean section. . Evaluation of scar thickness is done by ultrasound, but it is still debatable size of .
The integrity and thickness of the previous cesarean section scar of the lower uterine segment (LUS) assessed by ultrasound is a popular strategy that has been proposed to estimate the likelihood of uterine rupture or dehiscence that might occur spontaneously or during labor trial; this can be done alone or in combination with clinical factors . and measuring the scar in the mid-sagittal plane perpendicular . Incomplete healing of uterine scar after cesarean has been associated with adverse gynecological and obstetrical outcomes . This was a prospective cohort study of women with a singleton pregnancy and a single prior low-transverse CS. All participants underwent an evaluation of uterine scar by using transvaginal ultrasound at 11 to 13 weeks, including the presence of a scar defect and measurement of RMT; and a second evaluation at 35 to 38 weeks, combining both . While the secondary outcomes (as shown in figure 1) included the measurements of the anterior myometrial thickness(AMT) immediately adjacent to the scar ,the thickness of the myometrium bordering .
Incomplete healing of the scar is a recognized sequel of Cesarean section (CS) and may be associated with complications in later pregnancies. These complications can include scar pregnancy, a morbidly adherent placenta, scar dehiscence or rupture. . Standardized approach for imaging and measuring Cesarean section scars using ultrasonography . Analyzed were: shape scar thickness (thickening), continuity, border scar out, echoing the structure of the lower uterine segment and scar volume The study showed that scar thickness of 3.5 mm or .Scar thickness measurement by transvaginal sonography in late second trimester and third trimester in pregnant patients with previous cesarean section: Does sequential change in scar thickness with gestational age correlate with .
how to measure cesarean section
All participants underwent an evaluation of uterine scar by using transvaginal ultrasound at 11 to 13 weeks, including the presence of a scar defect and measurement of RMT; and a second evaluation at 35 to 38 weeks, combining both transvaginal and transabdominal ultrasound, for the measurement of LUS thickness.
The Cesarean birth rate is rising primarily due to the incidence of elective Cesarean sections (CS) which accounts for one third of CSs. . In 2010 Jastrow et al. conducted a meta-analysis of 12 articles on LUS thickness and risk of uterine scar defect and showed a strong association between the degree of LUS . In this Review we describe the .The other advantages of utilizing US for this diagnosis are its quick to perform, noninvasive, no radiation exposure and can be used for patient follow up. Hence, the rationale of the study was to explore the utility of US in scar thickness measurement and its value in predicting the scar integrity in term women with previous C-section.
The reliability of methods to predict the risks of uterine rupture in post LSCS pregnancies has been variable with sonographic measurement of scar thickness being the most sought after technique.[4,5] This may be one of the causes for a natural preference of repeat cesarean (both by the doctor and the patient) till certain reproducible and .
Many authors have tried to utilize transabdominal and transvaginal 2-D ultrasound to measure the scar thickness and detect the healing defects. . The cesarean scar was assessed using the . A significant association between a thin RMT as measured by transvaginal ultrasonography in the non-pregnant uterus after a first scheduled CS and the risk of uterine rupture or dehiscence at a subsequent delivery is suggested. Abstract Introduction Whether there is an association between residual myometrial thickness (RMT) after cesarean section (CS) . INTRODUCTION. A number of studies have used ultrasound imaging to describe Cesarean section (CS) scars 1-8; however, most have been carried out on non-pregnant women and findings are thus difficult to interpret in relation to the pregnant state.The appearance of CS scars on ultrasound examination may be clinically relevant, but there is limited evidence . To investigate whether the existing surgical technique for uterine closure at repeat lower segment Caesarean section (LSCS) can be modified to achieve adequate residual myometrial thickness (RMT) to ensure scar integrity and reduce complications in future pregnancy. Women with a significant scar defect at repeat LSCS had the anterior uterine wall .
Download Table | Uterine scar thickness measured by MRI and USG in patients being assessed for VBAC in grade I, grade II and grade III from publication: Comparative accuracy of magnetic resonance .Objective: To study the diagnostic accuracy of sonographic measurements of the lower uterine segment (LUS) thickness near term in predicting uterine scar defects in women with prior Caesarean section (CS). Data sources: PubMed, Embase, and Cochrane Library (1965-2009). Methods of study selection: Studies of populations of women with previous low transverse CS .The scar thickness obtained at late second and third trimester by transvaginal sonography (TVS) is shown in Table 2. The mean scar thickness when measured sono-graphically between 24 and 28 weeks was 4.53 ? 1.21 mm and beyond 36 weeks was 3.02 ? 0.92 mm. The scar thickness was maximum in the range of 4–5 mm (31 %) in
acompte. nm (sur somme due) payment on account , (sur salaire) advance. (=arrhes) deposit. (=versement régulier) instalment. un acompte de 100 euros 100 euros on .
measuring cesarean scar thickness|cesarean section scar measurement